Sign-it.
Simplified hospital admissions & insurance claim forms processing, boosting cash flow up to 75%.
About the product.
Sign‑It is an enterprise-grade claims and signature management system built for regulated hospital environments, designed to streamline pre-admission and billing workflows, reduce unbilled claims, and accelerate cash flow while improving accuracy and compliance. The system now handles over 500K processed claims worth more than €300M.
Sig-It is live in the major hospitals across Ireland, including Cork, Dublin, Galway, Limerick, and Tralee, helping more than 100K patients to relieve the stress of filling complicated insurance forms while optimising the hospital’s revenue cycle.
My role: Senior Product Designer
(Discovery, user research, strategy, information architecture, prototyping, design system, collaboration with engineering, mentoring)
Timeline: Mar 2023 – Apr 2024
Results so far.
%
Patient signatures captured
%
€1.4M more billing per week
%
Pre-admission forms completed
%
Improved Cashflow
Design approach.
Understand → Create ←→ Validate→ Deliver
The problem.
Hospitals were struggling with slow, error-prone, paper-based processes for managing claim forms and collecting patient signatures. Clerical officers often had to recomplete forms when patients forgot them, causing delays.
There was also no visibility into which patients had completed pre-admission steps before arriving, leading to inefficiencies, missed data, and delays in billing.
Unbilled claims were piling up, negatively impacting cash flow. A scalable, intuitive solution was urgently needed to streamline pre-admissions, signature collection, and claim processing.
Discovery & Research.
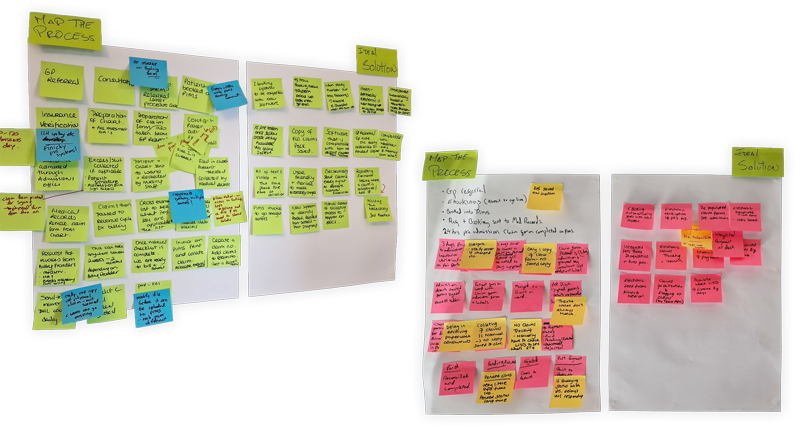
To begin, I led discovery sessions across multiple hospital sites with diverse stakeholders: clerical officers, billers, revenue cycle managers, IT staff, and third-party billers.
We mapped their workflows, pain points, and goals, uncovering hidden needs and interdependencies across roles.

These sessions helped shape a clear understanding of:
Q: Where did the delays happen?
A: Verifying policy details, missing signatures, and follow-up.
Q: Where did the errors originate?
A: Signing outside the dedicated area, procedure information incomplete, wrong patient details, e.g, DOB.
Q: What does each role need?
A: Clear way to identify when requests for changes have been fulfilled, automatic validation of minimum requirements, clear status of the claims and pre-admissions, and more.
Q: Identify the current business workflow for each persona of the claim collation process
A: We discovered that different hospitals have different business processes for capturing and collating claims that significantly impacted the quality.
Market research.
We also benchmarked against the only existing tool in Ireland, an older system used across hospitals. This provided a baseline of must-have features and design constraints.
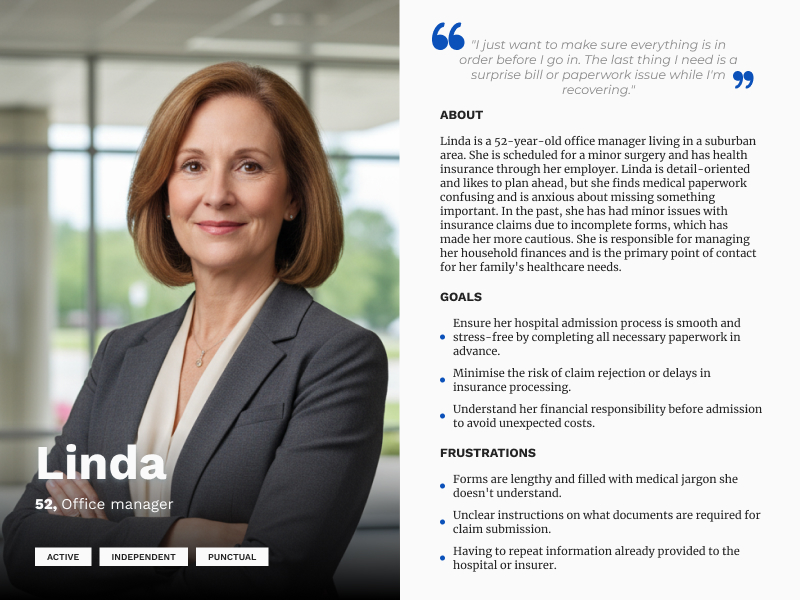
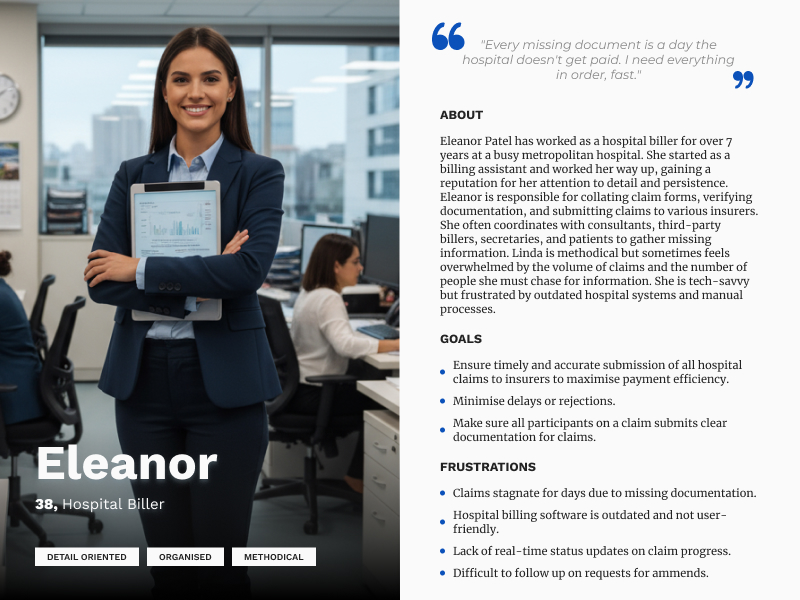
Personas & Mental Models.
Using the discovery insights, we created personas representing key user types: clerical staff, billers, consultants, and patients. Each had different levels of digital fluency and responsibilities. These personas anchored our UX decisions, ensuring we were solving real problems with empathy.
Instead of looking at personas in isolation, I used them to guide system-wide patterns. By mapping real mental models and uncovering process gaps, I identified where our product could create the most leverage, not just by improving individual workflows, but by streamlining handoffs, reducing uncertainty, and aligning expectations across teams.
Peripheral personas.
In addition, we’ve identified a set of secondary personas, such as consultants, receptionists, and insurers, who acted as supporting roles within the broader ecosystem.
| Persona | Role | Goals | Pain Points |
|---|---|---|---|
| Medical Billing Specialist (Billers) | Responsible for creating invoices and collating all documents for a claim. | Accurate and fast claim submission, handling pended, rejected, and partially paid claims. | Missing information, chasing up individuals for details, PMI queries. |
| Credit Control Specialist | Manages the financial aspect of claims post-PMI review. | Accurate reporting of paid, partially paid, and rejected claims, implement action mechanisms. | Incomplete information from PMIs, challenging PMIs, redirecting invoices to patients. |
| Patient | End-user who needs medical treatment. | Easy pre-admission process, understanding of costs and procedures. | Complexity in forms, uncertainty about insurance coverage. |
| Hospital Administrator | Manages hospital settings and policies. | Smooth system operation, set hospital-level rules for claims. | Complexity in managing multiple facilities, keeping up with policy changes. |
| Consultant/Specialist | Performs medical procedures. | Easy submission of their own invoices and any required additional forms. | Time-consuming paperwork, unclear submission processes. |
| Third-party Biller | External entity managing billing for consultants. | Efficient claim compilation for multiple consultants. | Keeping track of various forms and invoices, changes in hospital or PMI policies. |
| Insurer (PMI) Agent | Reviews and processes claims from hospitals. | Efficient and accurate claim processing. | Incomplete claims, discrepancies in documentation. |
| IT Administrator | Manages the technical aspects of the system. | Ensure system uptime, manage API settings. | Complexity in API integrations, system bugs or downtimes. |
| Customer Support Agent | Helps with queries from all users. | Quick resolution of user issues. | Lack of information on current claims, difficulty navigating the system. |
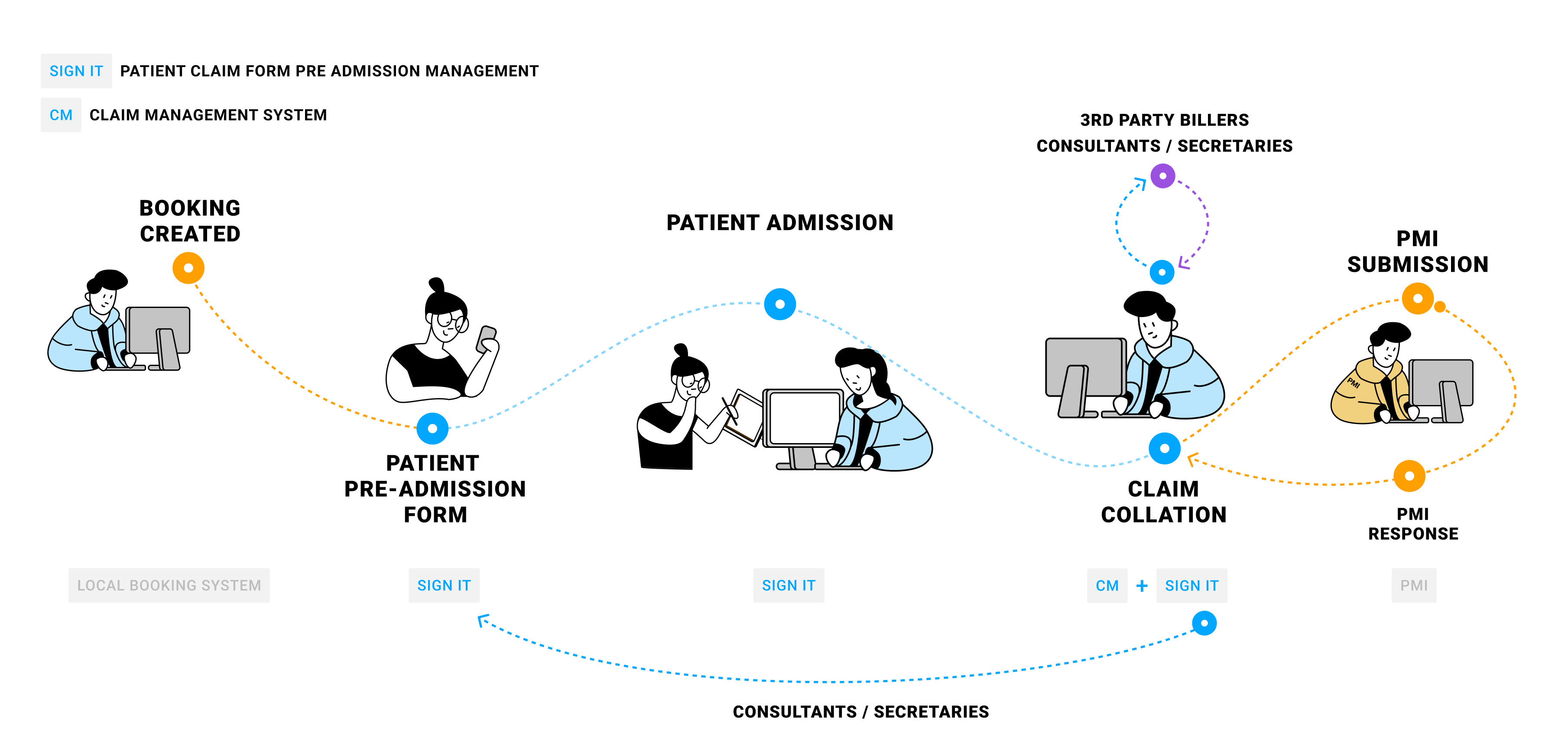
Mapping the journey.
Understand → Create ←→ Validate→ Deliver
Ideation and concept.
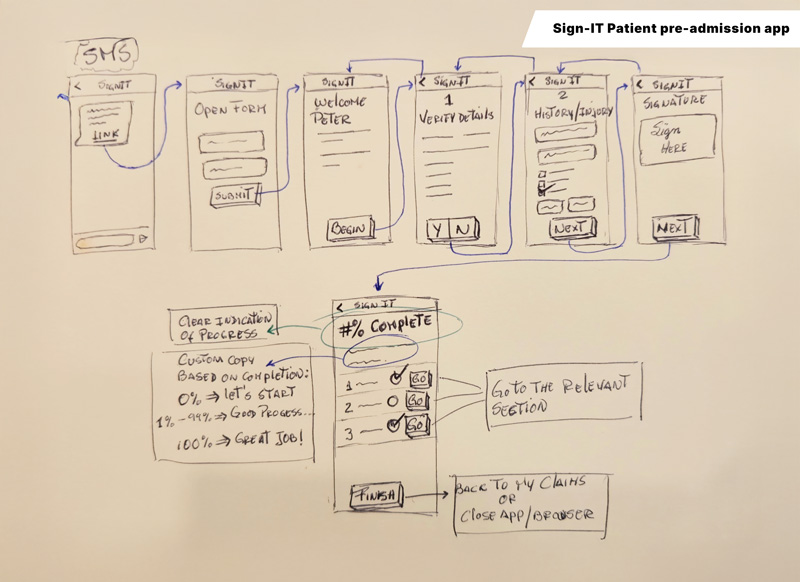
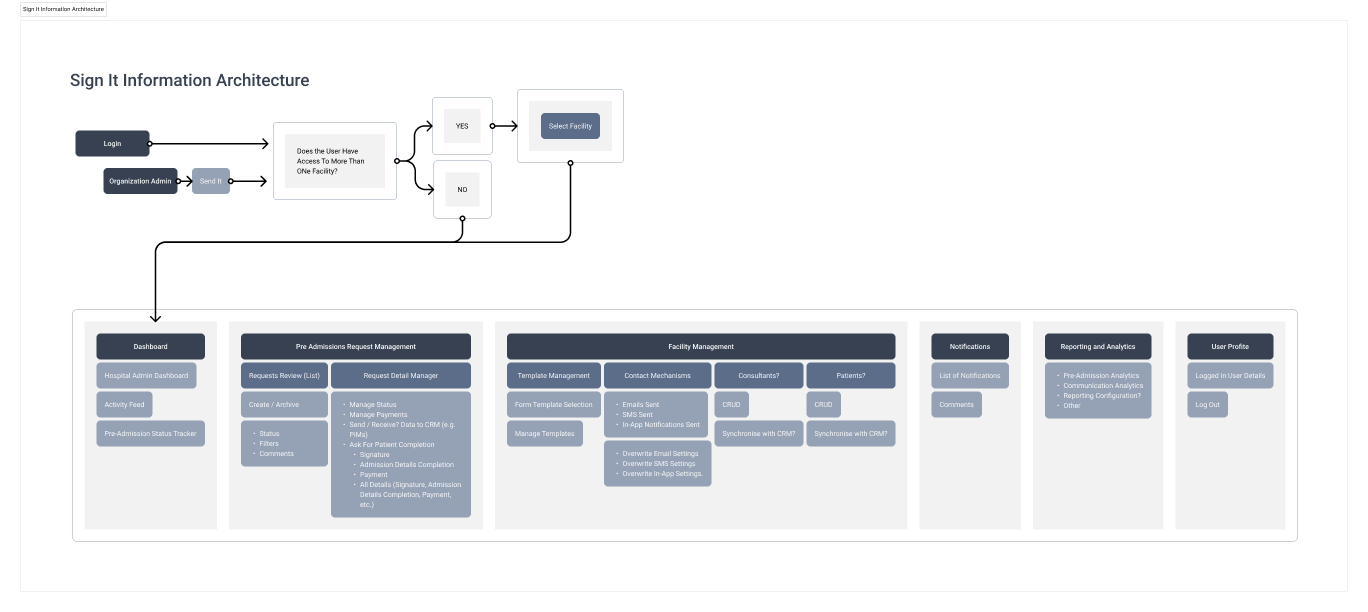
From here, I broke down the platform into digestible modules that became independent applications:
- Sign-It portal (Hospital).
- Claim management (Hospital).
- Consultant Portal (Consultants).
- Sign-It Pre-admission app (Patient).
- Signature capture Kiosk app (Patient & Hospital).
I transformed key workflows into epics and user stories, working closely with devs and PMs to ensure scope clarity. Each application had its own development cycle and Jira boards. As a. team, we’ve followed Agile practices.
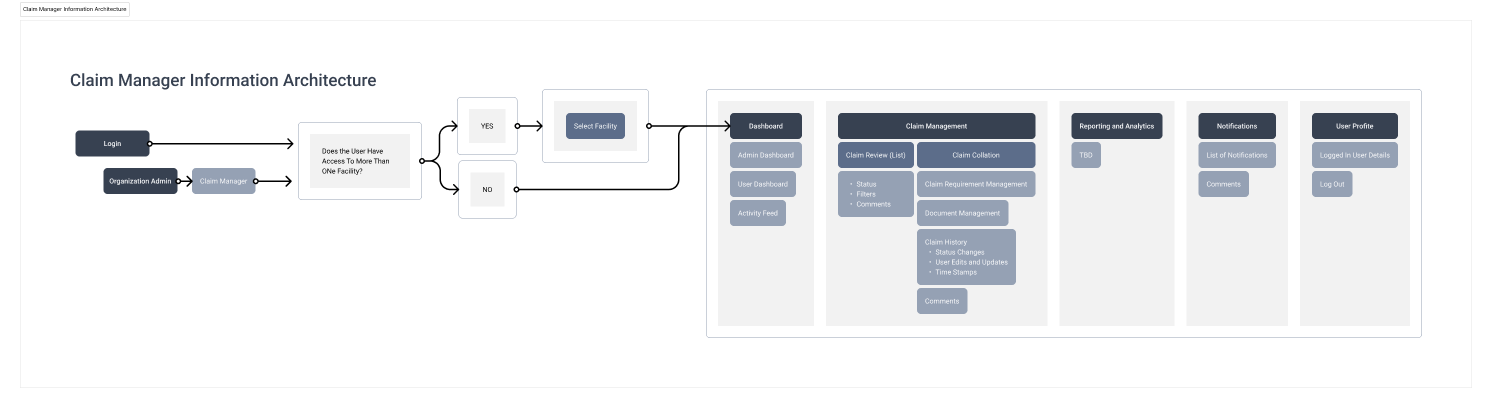
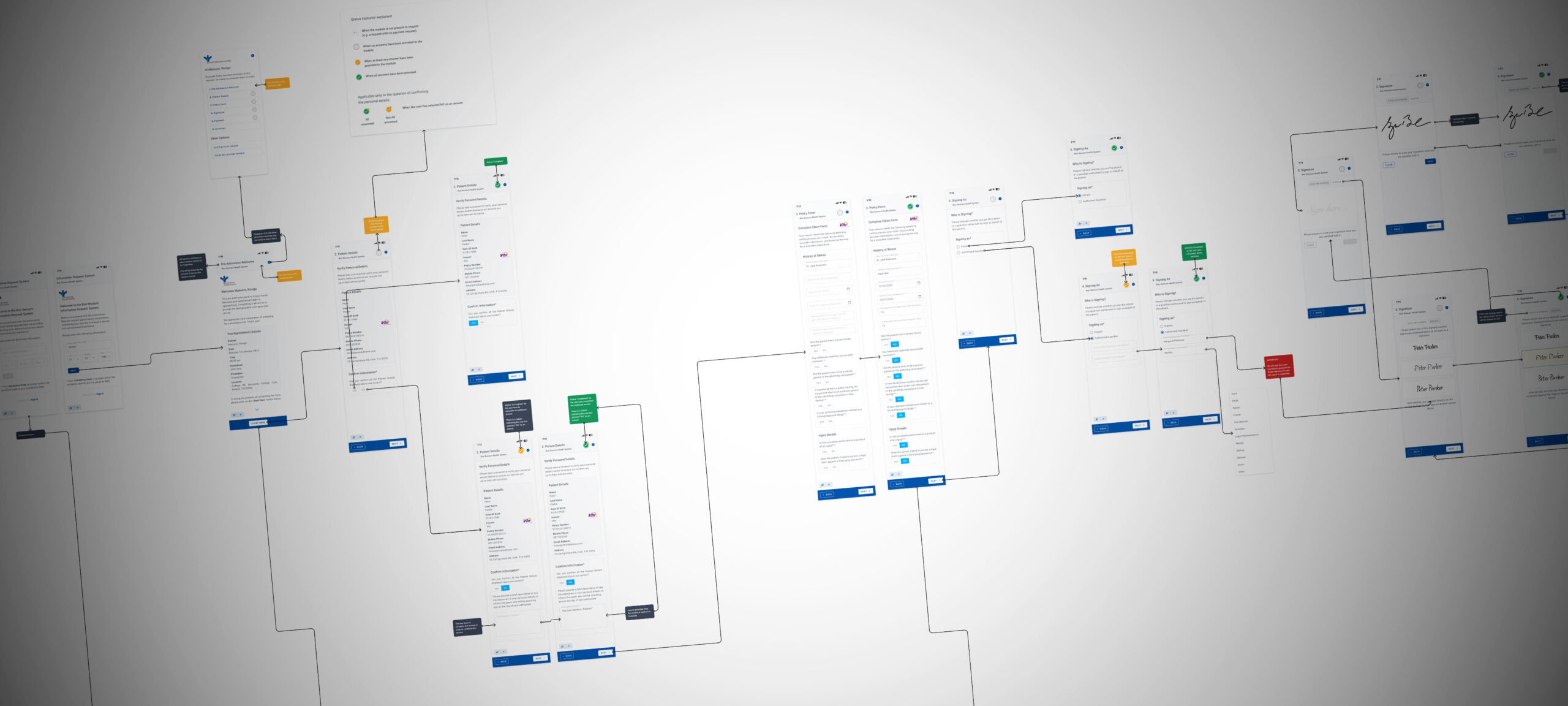
Information architecture.
Design & Prototyping.
Key design considerations included:
-
High-contrast colour schemes for CTAs and headers, supporting users with low vision and aligning with WCAG accessibility standards.
-
Larger-than-standard tap targets for all primary actions, ensuring usability for elderly and motor-impaired users across mobile, tablet, and kiosk.
-
Clear, step-by-step claim form flows, reducing errors and ensuring legal completeness in a medically sensitive context.
-
Consistent interaction patterns across modules to minimise training time and prevent user error.
-
Design decisions guided by compliance awareness, including audit traceability, secure signature handling, and alignment with GDPR and healthcare data protocols.
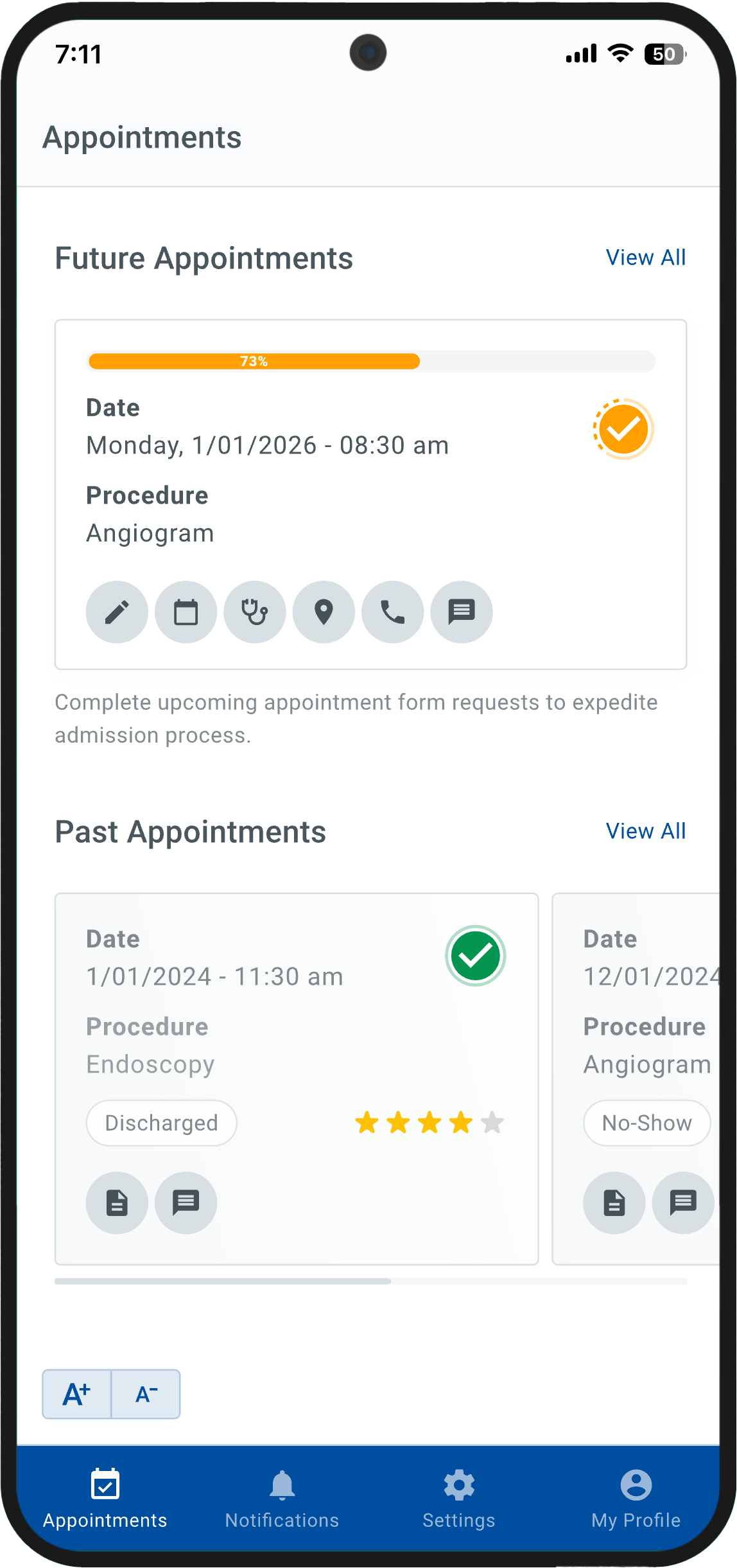
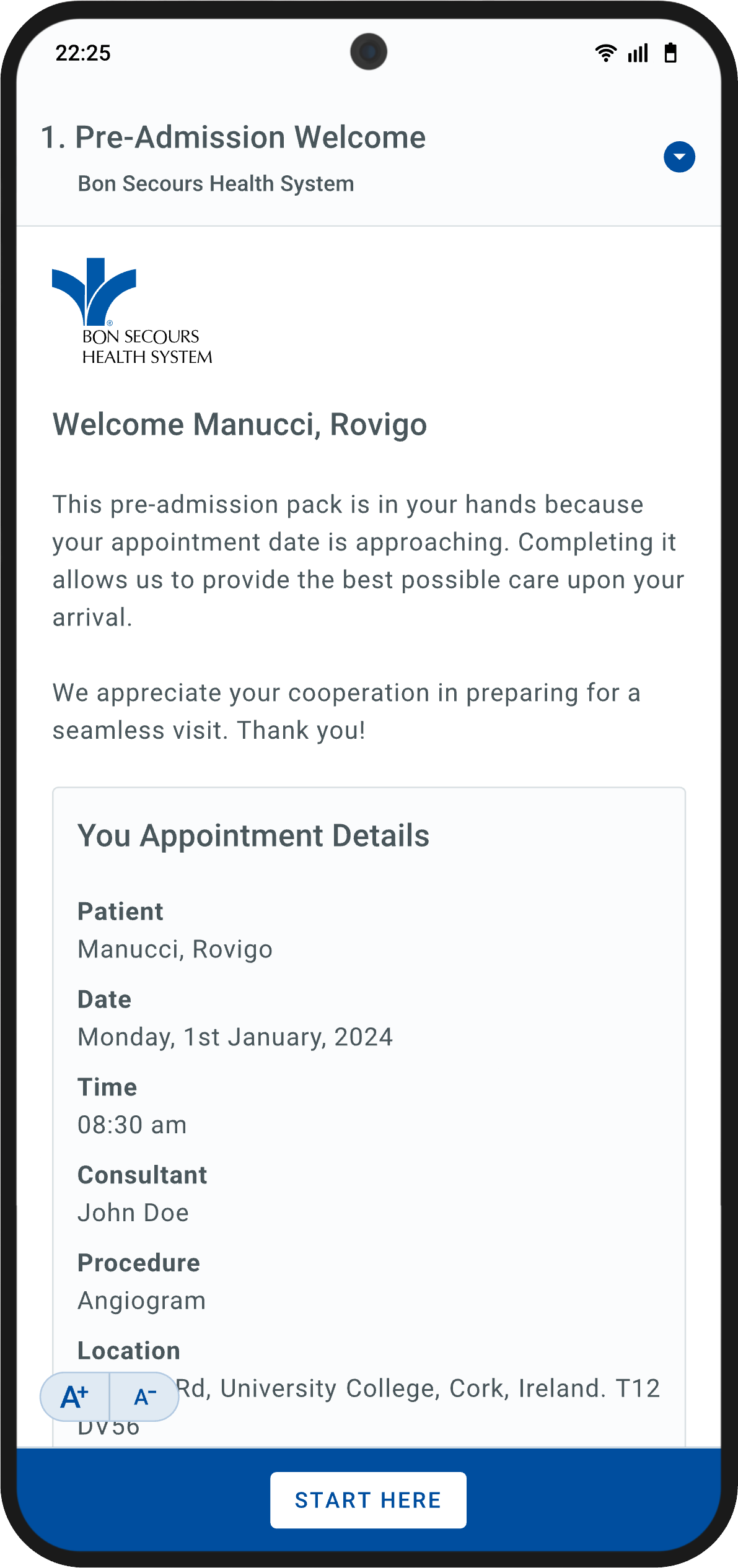
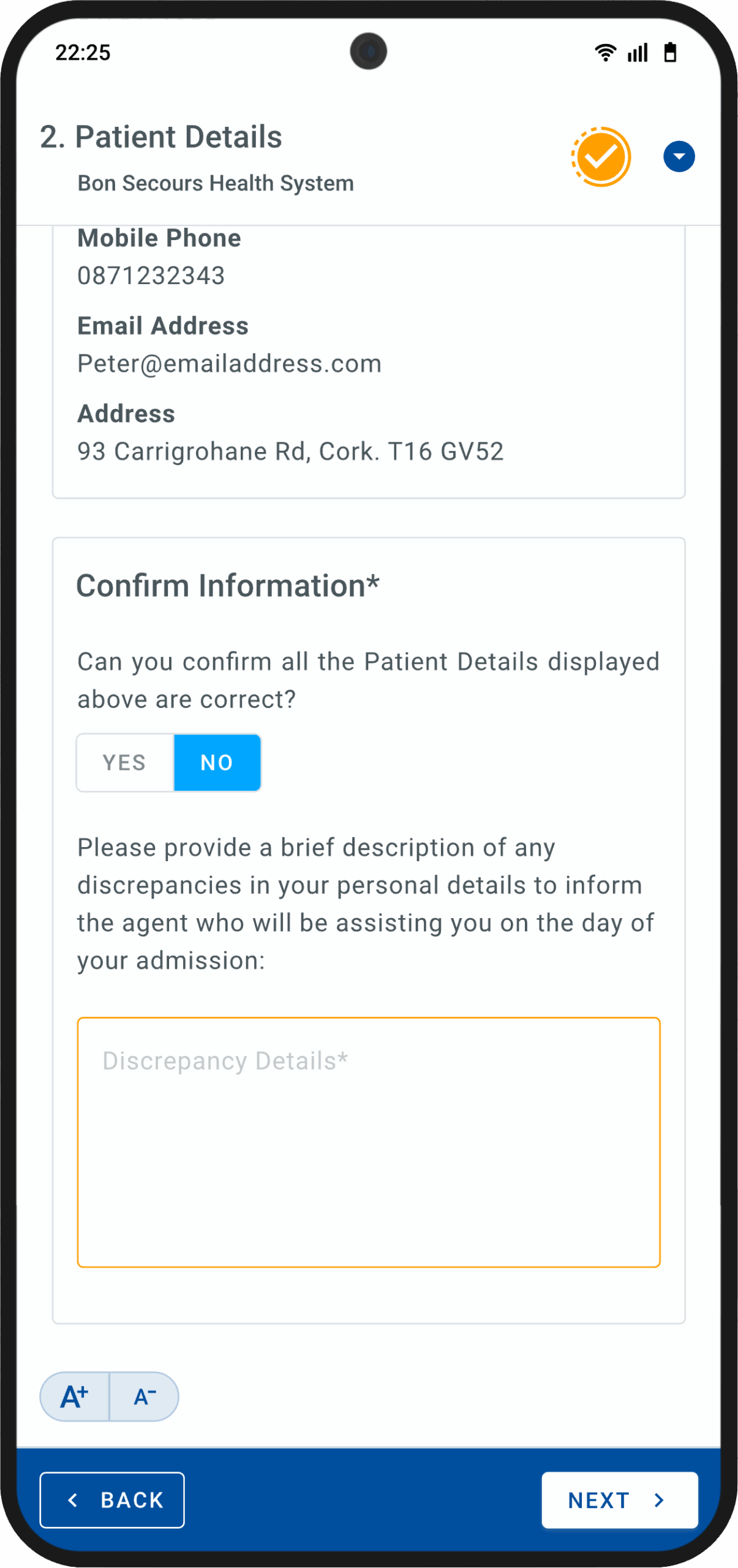
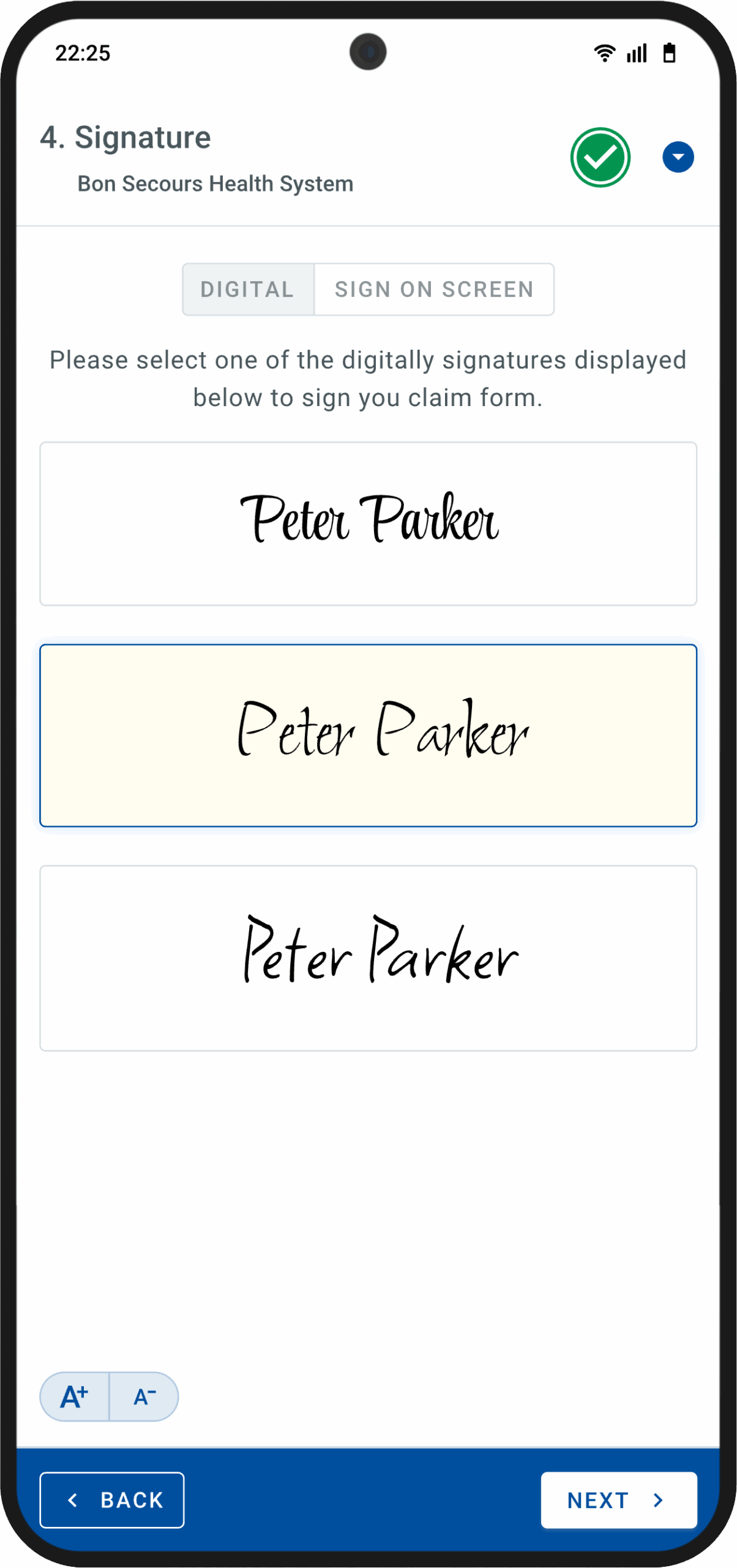
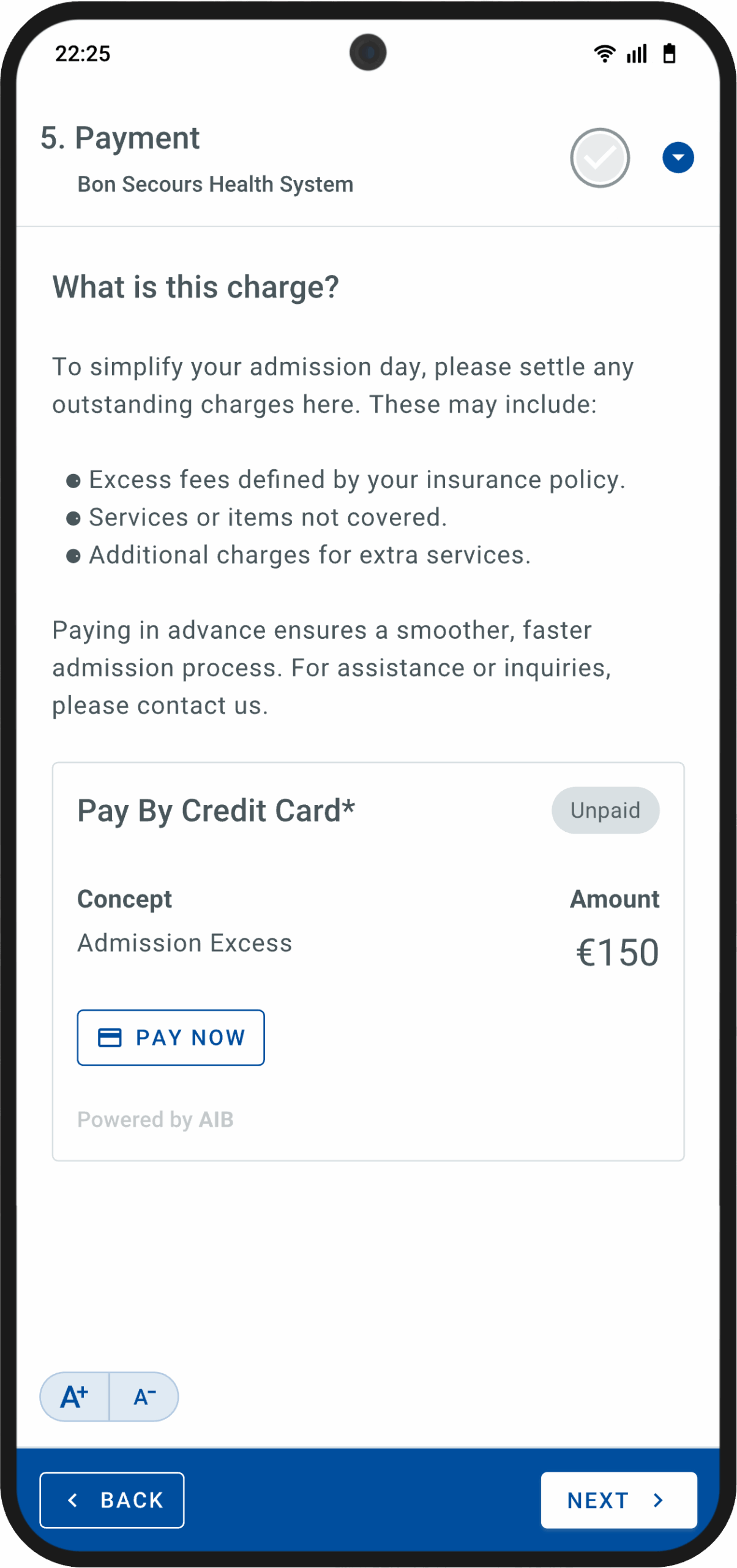
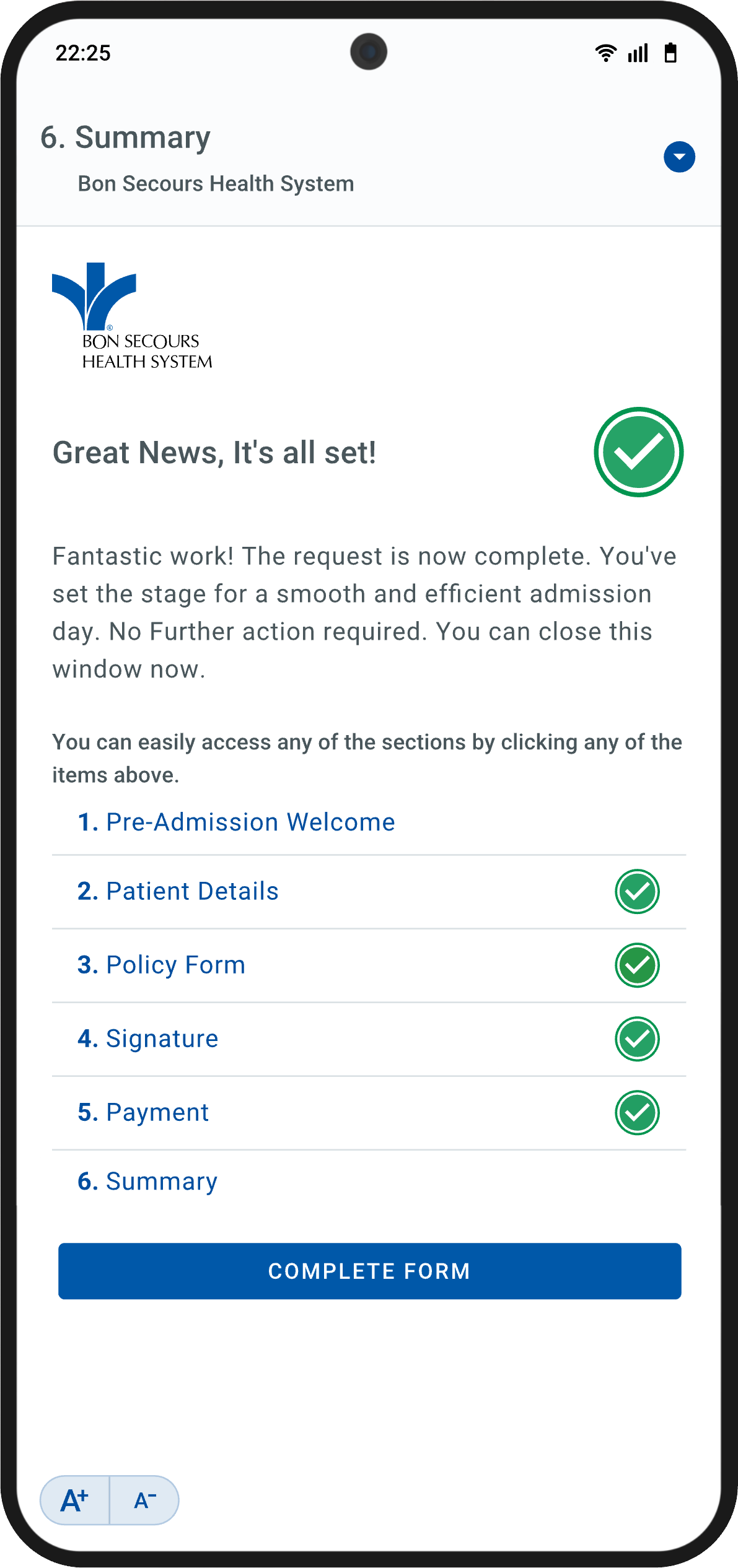
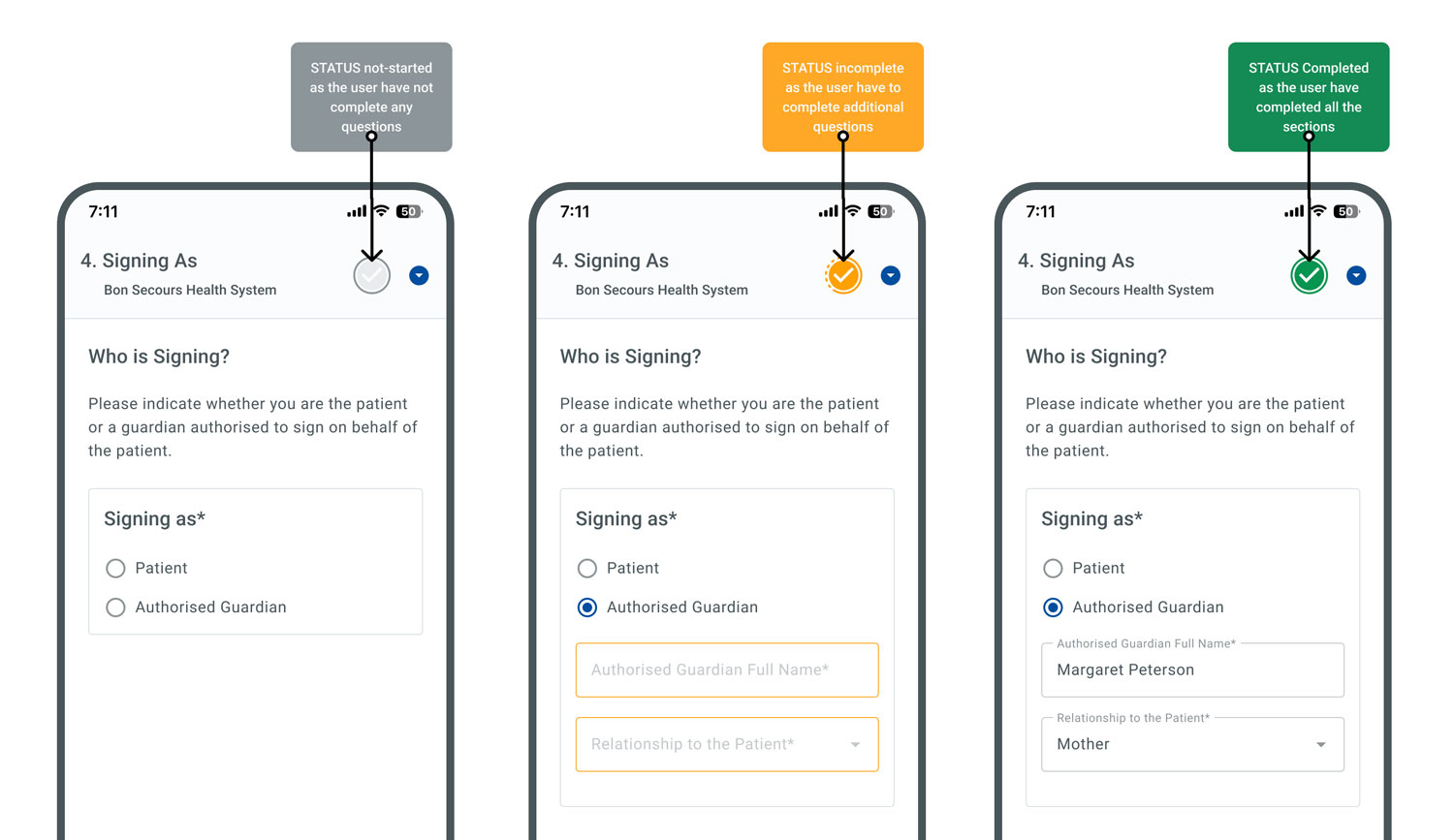
Sign-It patient app hi-fidelity mockups.
I moved quickly from low-fidelity sketches to high-fidelity prototypes in Figma, prioritising clarity, progressive disclosure, and reducing cognitive load. To support efficient development and UI consistency, I built a custom design system inspired by Material UI and adapted it to the needs of a regulated healthcare environment.
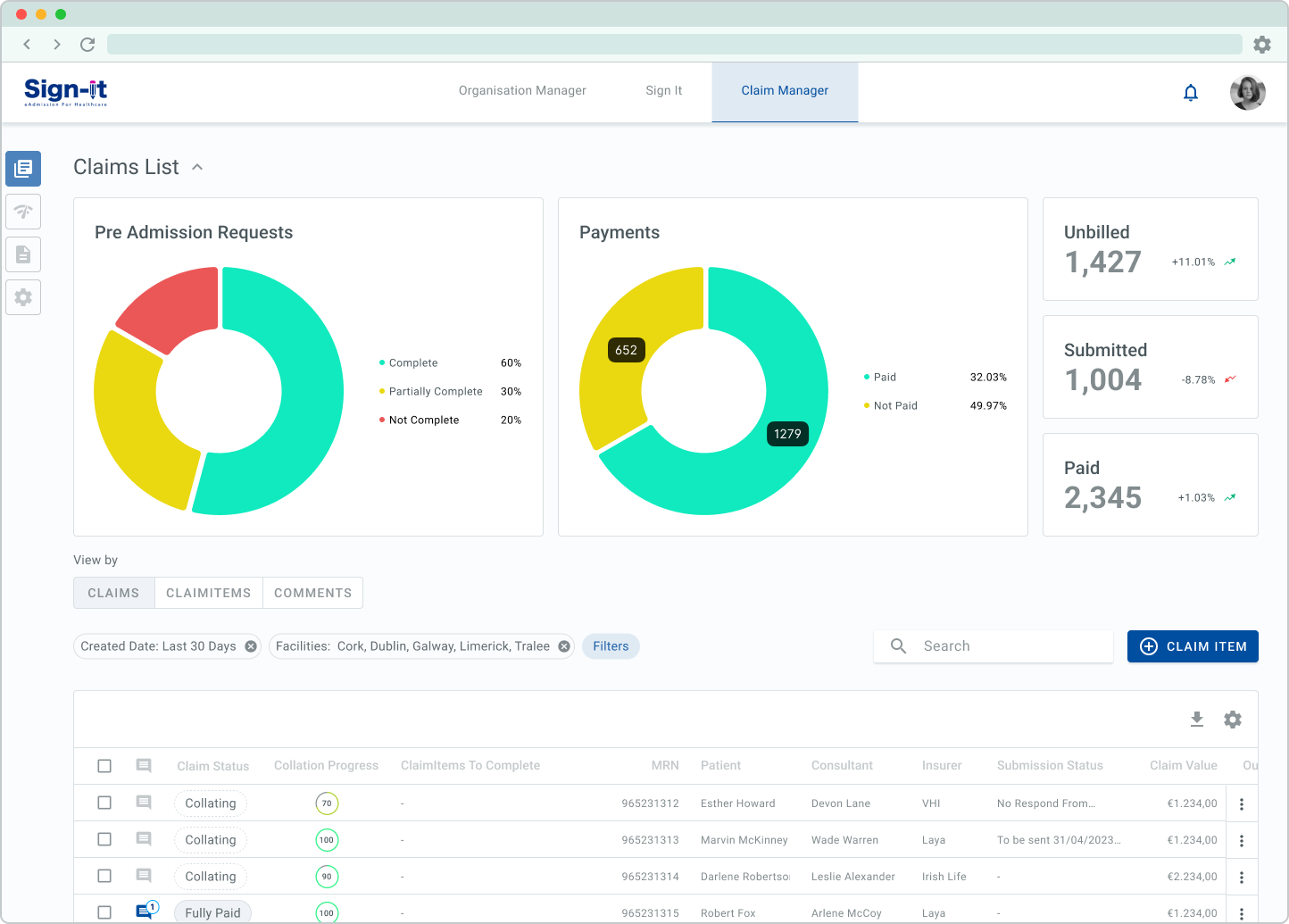
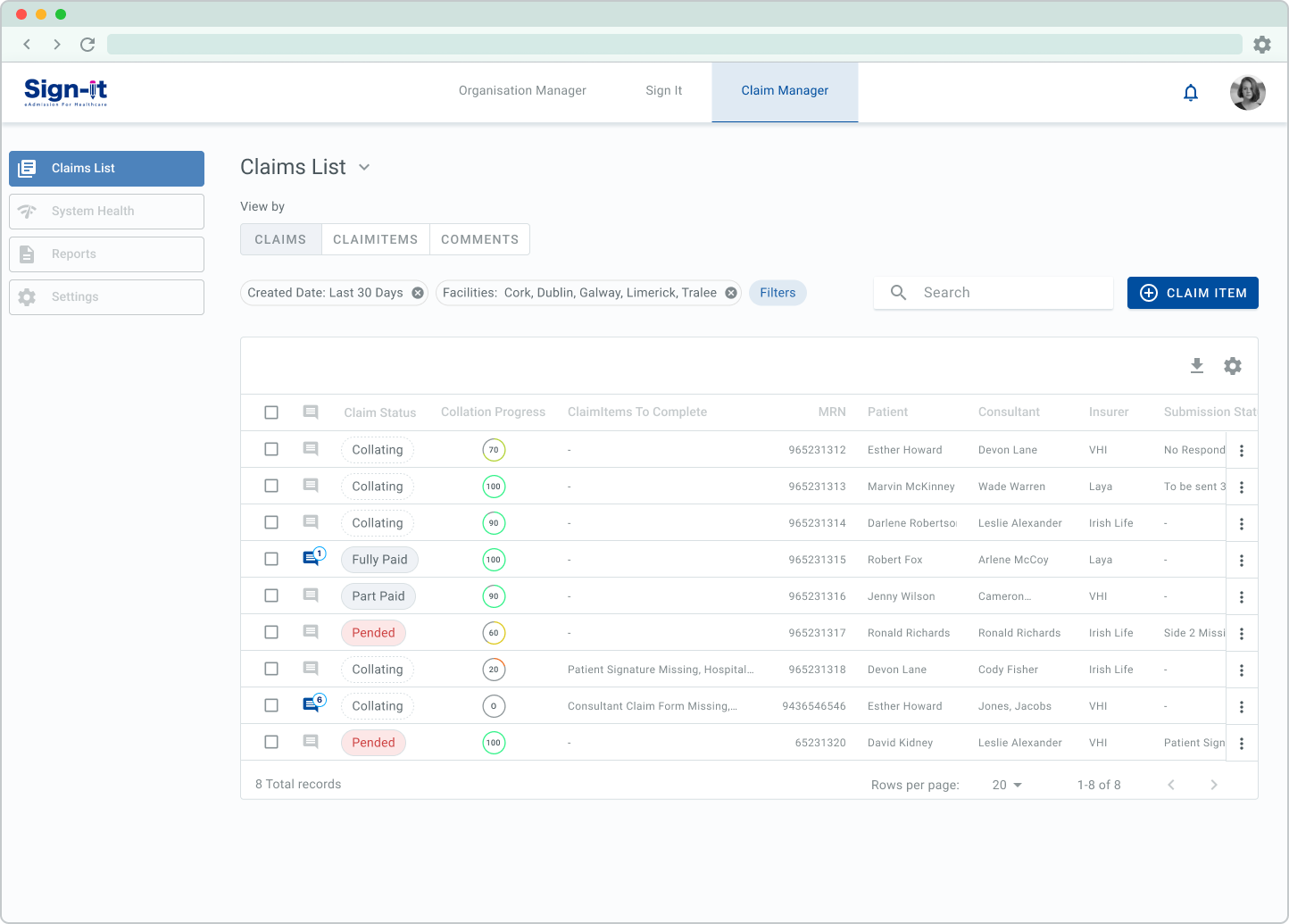
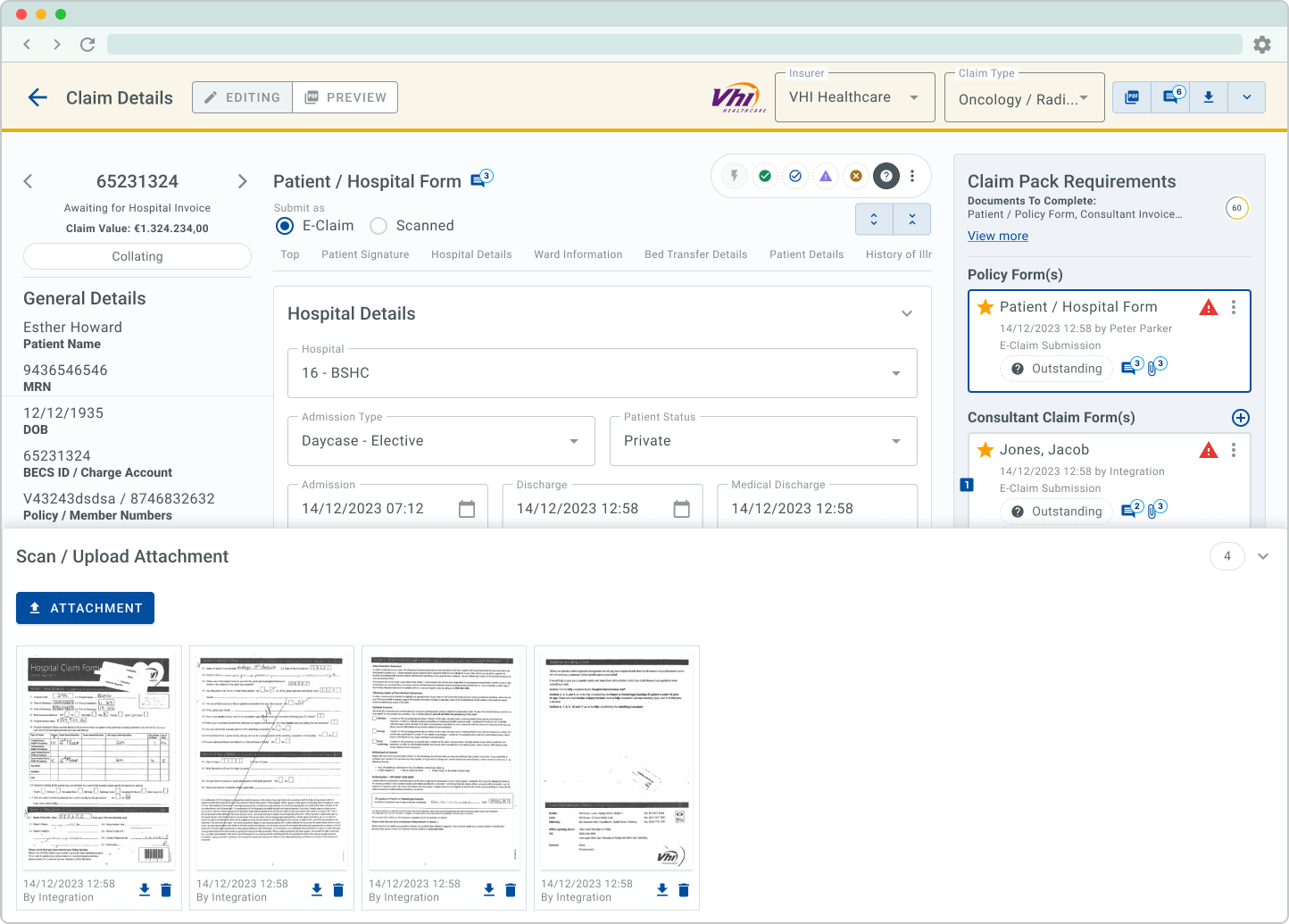
Claim list web app.
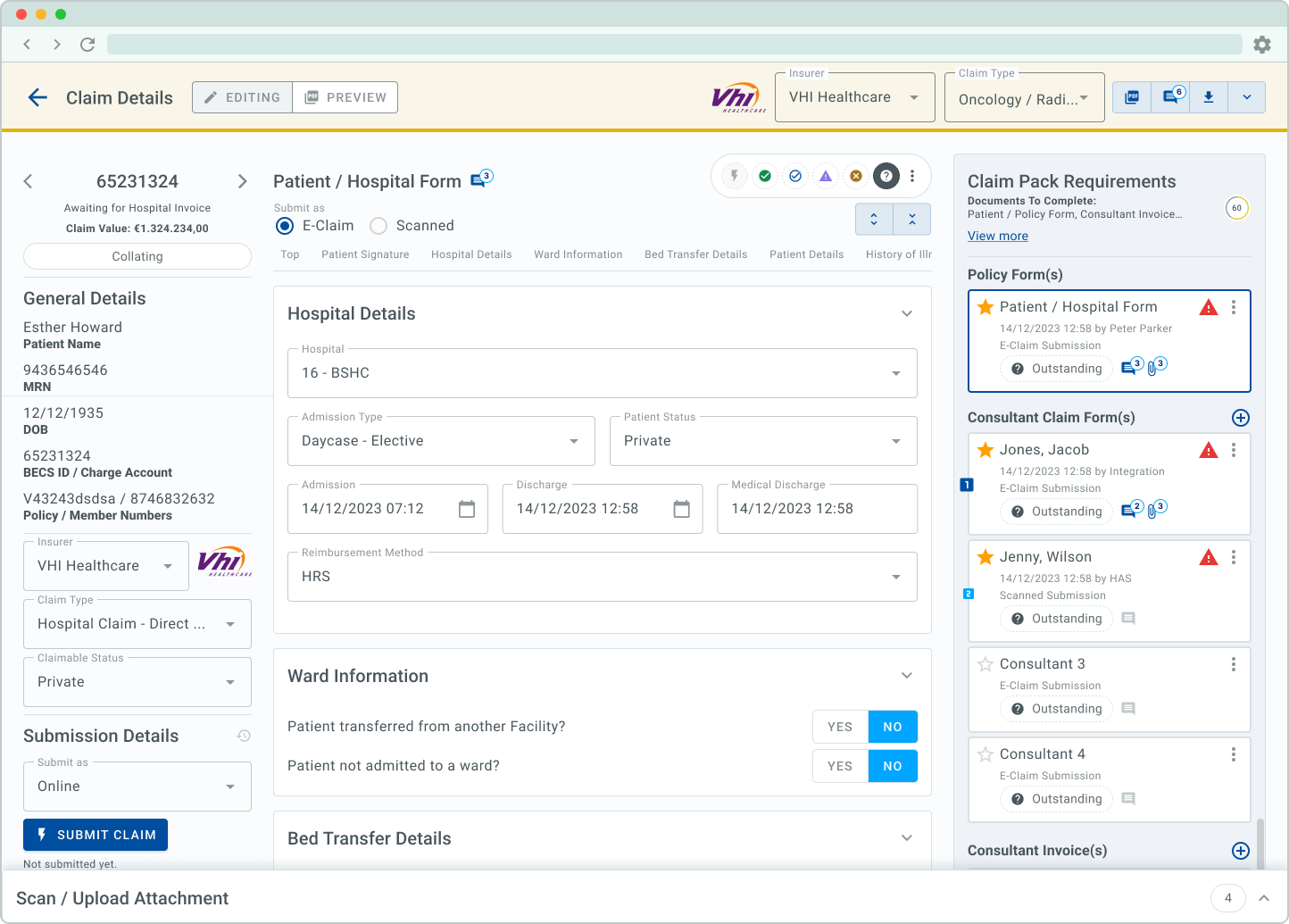
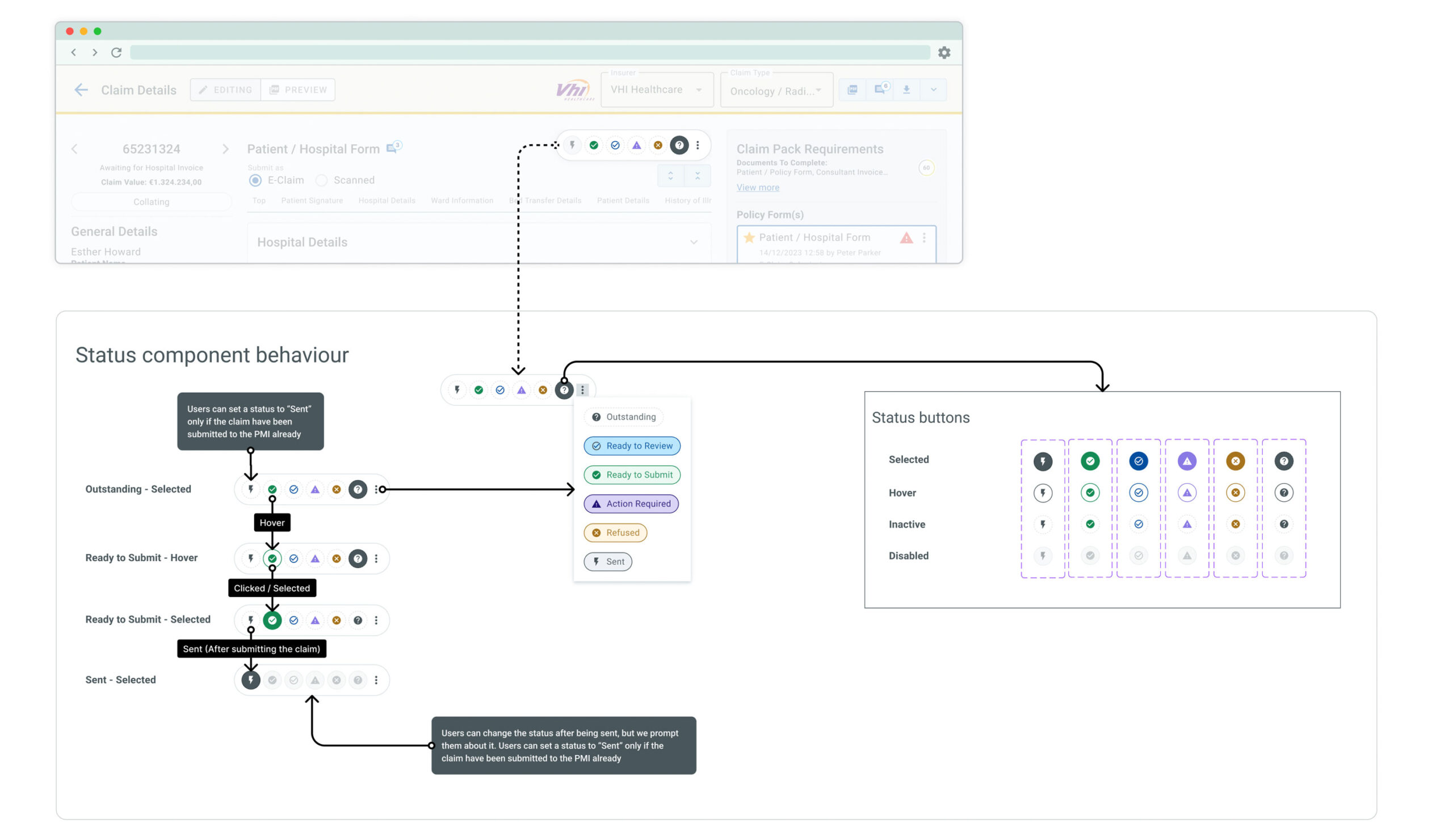
Claim details web app.
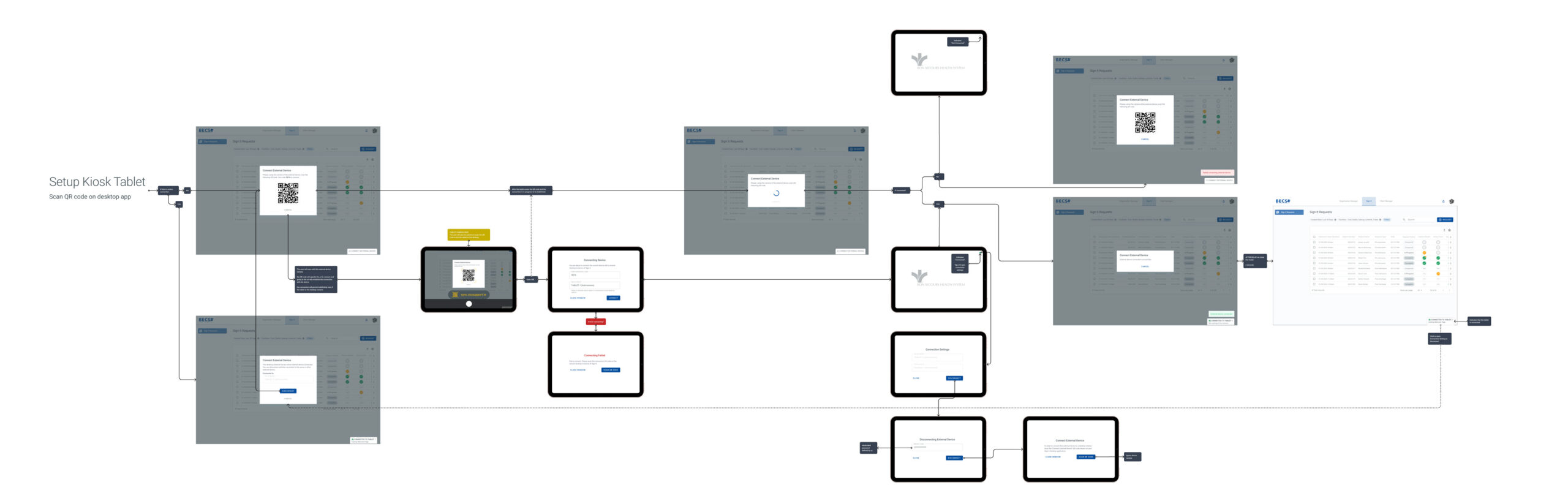
Kiosk tablet set up flow.
Before being used, each tablet kiosk needed to be securely linked to the system through a one-time setup process. This flow illustrates how staff scan a unique QR code from the desktop app, authenticate the device, and complete the pairing with a passcode to enable signature capture and claim form interactions.
Keeping an eye on the deliverables.
Understand → Create ←→ Validate→ Deliver
Testing & Iteration.
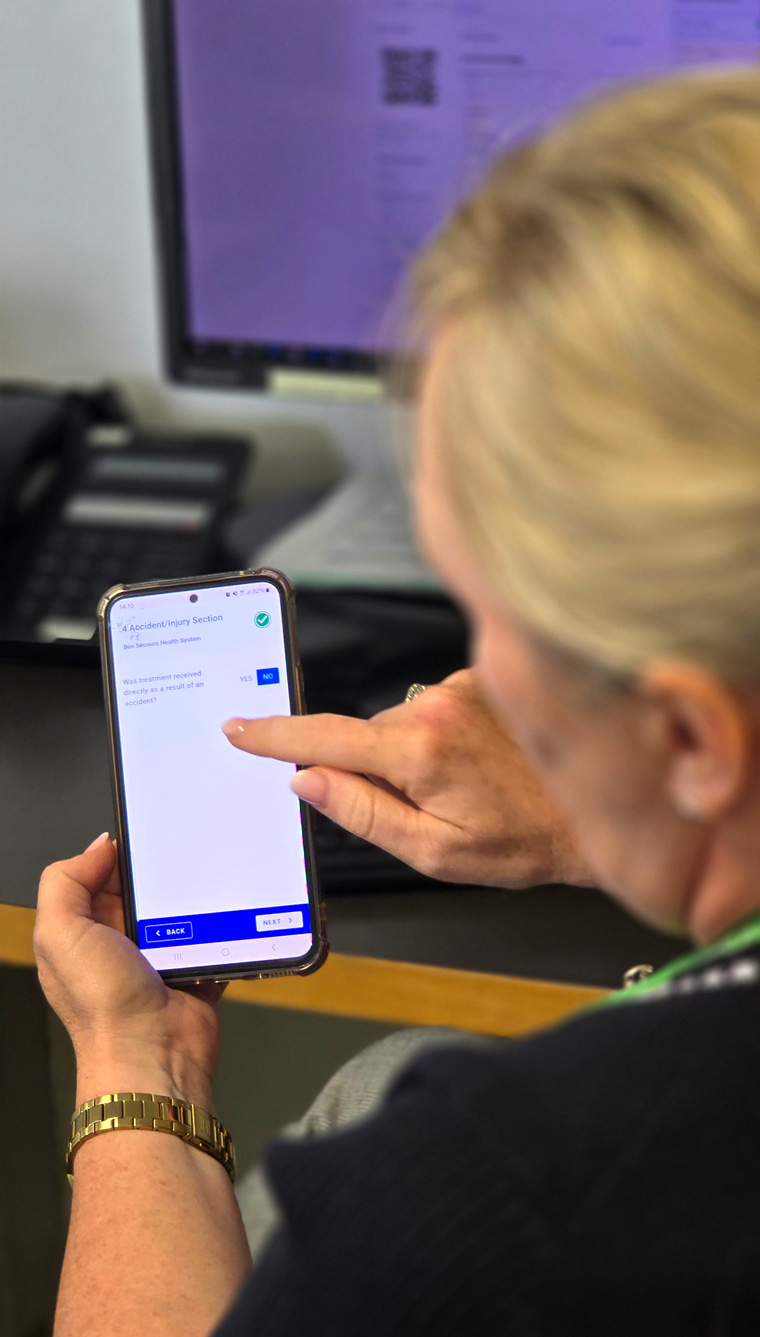
We ran ongoing iterative testing throughout the process. Once we had key flows solidified, we coordinated usability tests with:
- Billers and clerical officers who hadn’t seen the system before.
- Patients undergoing standard procedures, open to participating in friendly testing.
Our goal:
- First impressions: what users believed each screen was for.
- Task completion: how well they navigated flows without guidance.
- Observations on clickable and scroll patterns.
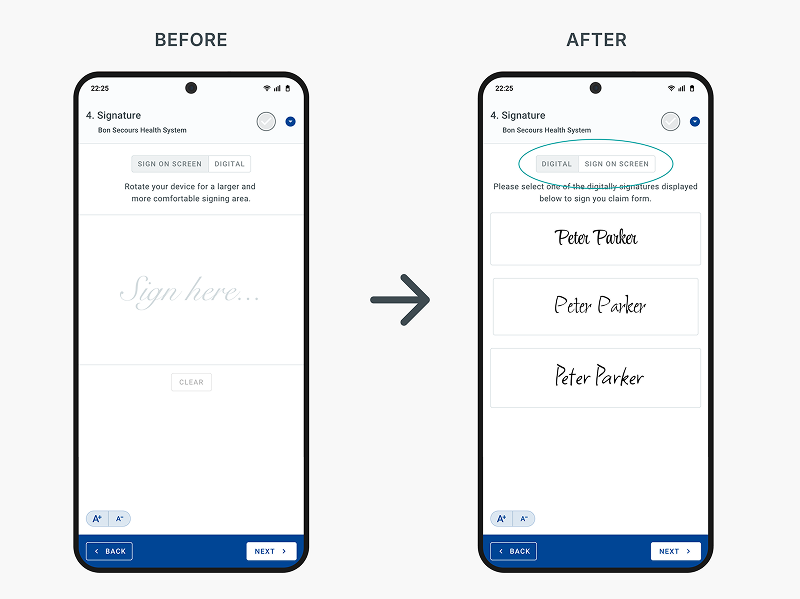
Huge win from the testing and observation sessions.
We offered two ways for patients to sign: on-screen or by selecting a digital signature. While we initially favored on-screen signing, mirroring the traditional paper method, we found that over 40% of patients, especially the elderly population, were being guided to choose the digital option due to difficulty signing. We quickly responded by reversing the toggle order and setting “Digital” as the default.
The update reduced signature-related friction and improved admission speed by an estimated 15–20%.
Understand → Create ←→ Validate→ Deliver
Handoff & Launch.
As a tightly-knit team, I was present during the full dev cycle. Handoff was seamless thanks to:
- Detailed Figma specs with notes.
- Story-level prototypes.
- Screen recordings with voice-over explanations.
Before each release, I helped to QA-test the staging environment:
- Flagged UI inconsistencies and bugs.
- Validated design implementation.
I also contributed to PM activities:
- Performed multiple pre-launch demos.
- Multi-session user trainings across sites (10–15 participants per session x ~5 sessions/day).
- Creation of PDF guides, crib sheets, and training videos for seamless onboarding.

Impact & Results.
Admission efficiency.
When forms aren’t completed in advance, the synced desktop and kiosk flow allows signatures to be captured in seconds and the full form completed in under a minute, thanks to a UI refined through ongoing user research.
%
Faster admissions
%
Faster Pre-admitted patients admissions
%
Patient signatures captured
Adoption of pre-admission forms.
Faster admissions were enabled by letting patients complete and sign forms before arrival, giving staff time to review and follow up. UX copy improvements based on feedback increased trust and completion rates.
%
Claim forms completed before admission
%
Claim forms completed before admission after ux copy improvements
Reduction in unbilled claims and better cashflow.
Features driven by user research, such as clear error indicators, intuitive filters, and the comment tool I championed to solve follow-up issues, led to higher claim quality. As a result, insurers reduced payment cycles from one month to one week, boosting hospital cash flow.
%
€1.4M more billing per week
%